Caudate nucleus
| Caudate nucleus | |
|---|---|
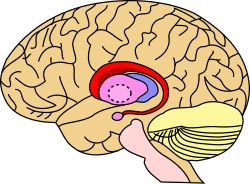 Caudate nucleus (in red) shown within the brain | |
Transverse cut of brain (horizontal section), basal ganglia is blue | |
| Details | |
| Part of | Dorsal striatum |
| Identifiers | |
| Latin | nucleus caudatus |
| MeSH | D002421 |
| NeuroNames | 226 |
| NeuroLex ID | birnlex_1373 |
| TA98 | A14.1.09.502 |
| TA2 | 5561 |
| FMA | 61833 |
| Anatomical terms of neuroanatomy | |
The caudate nucleus is one of the structures that make up the corpus striatum, which is part of the basal ganglia in the human brain.[1] Although the caudate nucleus has long been associated with motor processes because of its role in Parkinson's disease,[2][clarification needed][3] it also plays important roles in nonmotor functions, such as procedural learning,[4] associative learning,[5] and inhibitory control of action.[6] The caudate is also one of the brain structures that compose the reward system, and it functions as part of the cortico-basal ganglia-thalamo-cortical loop.[1]
Structure
[edit]
Along with the putamen, the caudate forms the dorsal striatum, which is considered a single functional structure; anatomically, it is separated by a large white-matter tract, the internal capsule, so it is sometimes also described as two structures—the medial dorsal striatum (the caudate) and the lateral dorsal striatum (the putamen). In this vein, the two are functionally distinct not because of structural differences, but merely because of the topographical distribution of function.
The caudate nuclei are near the center of the brain, sitting astride the thalamus. There is a caudate nucleus in each hemisphere of the brain. Each nucleus is C-shaped, with a wider "head" (caput in Latin) at the front, tapering to a "body" (corpus) and a "tail" (cauda). Sometimes a part of the caudate nucleus is called the "knee" (genu).[7] The caudate head receives its blood supply from the lenticulostriate artery; the tail of the caudate receives its blood supply from the anterior choroidal artery.[8]

The head and body of the caudate nucleus form part of the floor of the anterior horn of the lateral ventricle. The body travels briefly towards the back of the head; the tail then curves back toward the anterior, forming the roof of the inferior horn of the lateral ventricle. This means that a coronal section (on a plane parallel to the face) that cuts through the tail will also cross the body and head of the caudate nucleus.
Neurochemistry
[edit]The caudate is highly innervated by dopaminergic neurons that originate from the substantia nigra pars compacta (SNc). The SNc is in the midbrain and contains cell projections to the caudate and putamen, using the neurotransmitter dopamine.[9] There are also inputs from various association cortices.
Motor functions
[edit]Spatial mnemonic processing
[edit]The caudate nucleus integrates spatial information with motor behavior formulation. Selective impairment of spatial working memory in subjects with Parkinson's disease and the knowledge of the disease's impact on the amount of dopamine supplied to the striatum have linked the caudate nucleus to spatial and nonspatial mnemonic processing. Spatially dependent motor preparation has been linked to the caudate nucleus through event-related fMRI analysis techniques. Activity in the caudate nucleus was demonstrated to be greater during tasks featuring spatial and motoric memory demands than those that involved nonspatial tasks.[10] Specifically, spatial working memory activity has been observed, via fMRI studies of delayed recognition, to be greater in the caudate nucleus when the activity immediately preceded a motor response. These results indicate that the caudate nucleus could be involved in coding a motor response. With this in mind, the caudate nucleus could be involved in the recruitment of the motor system to support working memory performance by the mediation of sensory-motor transformations.[11]
Directed movements
[edit]The caudate nucleus contributes importantly to body and limbs posture and the speed and accuracy of directed movements. Deficits in posture and accuracy during paw-usage tasks were observed after the removal of caudate nuclei in cats. A delay in initiating performance and the need to shift body position constantly were both observed in cats after partial removal of the nuclei.[12]
In monkeys, after the application of cocaine to the caudate nucleus and the resulting lesions produced, there was a "leaping or forward movement". Because of its association with damage to the caudate, this movement demonstrates the inhibitory nature of the caudate nucleus. The "motor release" caused by this procedure indicates that the caudate nucleus inhibits the tendency for an animal to move forward without resistance.[13]
Cognitive functions
[edit]Goal-directed action
[edit]A review of neuroimaging studies, anatomical studies of caudate connectivity, and behavioral studies reveals a role for the caudate in executive functioning. A study of Parkinson's patients (see below) may also contribute to a growing body of evidence.
A two-pronged approach of neuroimaging (including PET and fMRI) and anatomical studies expose a strong relationship between the caudate and cortical areas associated with executive functioning: "non-invasive measures of anatomical and functional connectivity in humans demonstrate a clear link between the caudate and executive frontal areas."[14]
Meanwhile, behavioral studies provide another layer to the argument: recent studies suggest that the caudate is fundamental to goal-directed action, that is, "the selection of behavior based on the changing values of goals and a knowledge of which actions lead to what outcomes."[14] One such study presented rats with levers that triggered the release of a cinnamon flavored solution. After the rats learned to press the lever, the researchers changed the value of the outcome (the rats were taught to dislike the flavor either by being given too much of the flavor, or by making the rats ill after drinking the solution) and the effects were observed. Normal rats pressed the lever less frequently, while rats with lesions in the caudate did not suppress the behavior as effectively. In this way, the study demonstrates the link between the caudate and goal-directed behavior; rats with damaged caudate nuclei had difficulty assessing the changing value of the outcome.[14] In a 2003-human behavioral study, a similar process was repeated, but the decision this time was whether or not to trust another person when money was at stake.[15] While here the choice was far more complex––the subjects were not simply asked to press a lever, but had to weigh a host of different factors––at the crux of the study was still behavioral selection based on changing values of outcomes.
In short, neuroimagery and anatomical studies support the assertion that the caudate plays a role in executive functioning, while behavioral studies deepen our understanding of the ways in which the caudate guides some of our decision-making processes.
Memory
[edit]The dorsal-prefrontal cortex subcortical loop involving the caudate nucleus has been linked to deficits in working memory, specifically in schizophrenic patients. Functional imaging has shown activation of this subcortical loop during working memory tasks in primates and healthy human subjects. The caudate may be affiliated with deficits involving working memory from before illness onset as well. Caudate nucleus volume has been found to be inversely associated with perseverative errors on spatial working memory tasks.[16][17]
The amygdala sends direct projections to the caudate nucleus. Both the amygdala and the caudate nucleus have direct and indirect projections to the hippocampus. The influence of the amygdala on memory processing in the caudate nucleus has been demonstrated with the finding that lesions involving the connections between these two structures "block the memory-enhancing effects of oxotremorine infused into the caudate nucleus". In a study involving rats given water-maze training, the caudate nucleus was discovered to enhance memory of visually cued training after amphetamine was infused post-training into the caudate.[18]
Learning
[edit]In a 2005 study, subjects were asked to learn to categorize visual stimuli by classifying images and receiving feedback on their responses. Activity associated with successful classification learning (correct categorization) was concentrated to the body and tail of the caudate, while activity associated with feedback processing (the result of incorrect categorization) was concentrated to the head of the caudate.[19]
Sleep
[edit]Bilateral lesions in the head of the caudate nucleus in cats were correlated with a decrease in the duration of deep slow wave sleep during the sleep-wakefulness cycle. With a decrease in total volume of deep slow wave sleep, the transition of short-term memory to long-term memory may also be affected negatively.[20]
However, the effects of caudate nuclei removal on the sleep–wakefulness pattern of cats have not been permanent. Normalization occurs by three months after caudate nuclei ablation. This discovery may be due to the inter-related nature of the roles of the caudate nucleus and the frontal cortex in controlling levels of central nervous system activation. The cats with caudate removal, although permanently hyperactive, had a significant decrease in rapid eye movement sleep (REMS) time, which lasted about two months. However, afrontal cats had a permanent decrease in REMS time and only a temporary period of hyperactivity.[21]
Contrasting with associations between "deep", REM sleep and the caudate nucleus, a study involving EEG and fMRI measures during human sleep cycles has indicated that the caudate nucleus demonstrates reduced activity during non-REM sleep across all sleep stages.[22] Additionally, studies of human caudate nuclei volume in congenital central hypoventilation syndrome (CCHS) subjects established a correlation between CCHS and a significant reduction in left and right caudate volume. CCHS is a genetic disorder that affects the sleep cycle due to a reduced drive to breathe. Therefore, the caudate nucleus has been suggested to play a role in human sleep cycles.[23]
Emotion
[edit]The caudate nucleus has been implicated in responses to visual beauty, and has been suggested as one of the "neural correlates of romantic love".[24][25]
Approach-attachment behavior and affect are also controlled by the caudate nucleus. Cats with bilateral removal of the caudate nuclei persistently approached and followed objects, attempting to contact the target, while exhibiting a friendly disposition by the elicitation of treading of the forelimbs and purring. The magnitude of the behavioral responses was correlated to the extent of the removal of the nuclei. Reports of human patients with selective damage to the caudate nucleus show unilateral caudate damage resulting in loss of drive, obsessive-compulsive disorder, stimulus-bound perseverative behavior, and hyperactivity. Most of these deficits can be classified as relating to approach-attachment behaviors, from approaching a target to romantic love.[12]
Language
[edit]Neuroimaging studies reveal that people who can communicate in multiple languages activate exactly the same brain regions regardless of the language. A 2006 publication studies this phenomenon and identifies the caudate as a center for language control. In perhaps the most illustrative case, a trilingual subject with a lesion to the caudate was observed. The patient maintained language comprehension in her three languages, but when asked to produce language, she involuntarily switched between the three languages. In short, "these and other findings with bilingual patients suggest that the left caudate is required to monitor and control lexical and language alternatives in production tasks."[26][27]
Local shape deformations of the medial surface of the caudate have been correlated with verbal learning capacity for females and the number of perseverance errors on spatial and verbal fluency working memory tasks for males. Specifically, a larger caudate nucleus volume has been linked with better verbal fluency performance.[16]
A neurological study of glossolalia showed a significant reduction in activity in the left caudate nucleus during glossolalia compared to singing in English.[28]
Threshold control
[edit]The brain contains large collections of neurons reciprocally connected by excitatory synapses, thus forming large network of elements with positive feedback. It is difficult to see how such a system can operate without some mechanism to prevent explosive activation. There is some indirect evidence[29] that the caudate may perform this regulatory role by measuring the general activity of cerebral cortex and controlling the threshold potential.
Clinical significance
[edit]Caudate stroke
[edit]Strokes can occur in the caudate nucleus and studies of patients with these kinds of strokes followed the introduction and widespread availability of computed tomography (CT) scanning in the 1970s and early 1980s.[30][31] Major studies of caudate strokes have included Stein et al. (1984),[32] Weisberg et al. (1984),[33] Mendez et al. (1989),[34] Caplan et al. (1990),[35] Caplan & Helgason (1995),[36] Bokura & Robinson (1997),[37] Kumral et al. (1999),[38] Gnanashanmugam (2011),[39] and Kumral et al. (2023).[40][30][31] A number of literature reviews on caudate nucleus strokes have been published,[30][31][36][41][39] as well as a 1994 meta-analysis of basal ganglia lesions that included analysis of caudate lesions (Bhatia & Marsden, 1994).[42] Caudate strokes are rare, representing only 1% of all strokes in one population of about 3,000 stroke patients.[43][38] Caudate hemorrhages account for about 7% of all intracerebral hemorrhages.[30] Research on caudate strokes has consisted of small clinical series of patients and case reports.[31][30] A 2002 review described 108 patients with 119 caudate infarcts that had been characterized, with three of the largest series having a total of 64 patients.[31] In the 1994 meta-analysis, there were 43 patients with lesions confined to the caudate nucleus and 129 patients with lesions involving both the caudate and other structures, with 172 patients in total.[42]
Caudate nucleus strokes can be diagnosed with CT or magnetic resonance imaging (MRI) scanning.[31][36] They are a type of subcortical stroke and are classified as ischemic (infarcts) or hemorrhagic.[30][41] In one series of patients, 80% of strokes were ischemic and 20% were hemorrhagic.[39][38] Caudate infarcts can be lacunar infarcts, which are small and are due to a single perforating artery occlusion, or can be striatocapsular (caudate–putamen–internal capsule) infarcts, which are larger and are due to multiple perforating artery occlusion.[44][45] Caudate nucleus strokes infrequently affect only the caudate, but usually also involve neighboring areas like the anterior portion of the putamen, adjacent anterior limb of the internal capsule, adjacent corona radiata white matter, and globus pallidus.[30][42] About 25 to 30% of lesions are confined exclusively to the caudate.[42][31][30][36] Caudate strokes are usually unilateral, but can also be bilateral, affecting both the left and right caudate nuclei.[31][30] In the 1994 meta-analysis, 90% of isolated caudate infarcts were unilateral and 10% were bilateral.[42] Small vessel disease or penetrating-branch disease is a major mechanism of caudate strokes.[30][41] Major risk factors and causes of caudate infarcts include hypertension, hypercholesterolemia, diabetes mellitus, previous myocardial infarct, cigarette smoking, large artery lesions, rupture of internal carotid artery aneurysms, rupture of arteriovenous malformations, cardiac embolism, and carotid artery stenosis and occlusion.[30][41] Less common risk factors may include non-valvular atrial fibrillation, myocardial dyskinesia, cardiac aneurysm with a mural thrombus, syphilis, Hodgkin's lymphoma, and Moyamoya disease.[30][41] Additionally, a case report of lacunar infarction of the caudate and adjacent structures due to high-dose oral methylphenidate use has been published.[46][47]
Caudate nucleus strokes have been associated with a variety of clinical symptoms.[12][31][30] In studies of patients with caudate infarcts, frequently occurring symptoms have included dysarthria or dysphonia (61–86%), motor weakness (40–100%), and cognitive/behavioral abnormalities (39–78%), including abulia (26–48%), agitation (29%), restlessness, hyperactivity, disinhibition (9–11%), executive dysfunction or frontal system abnormalities (26%), memory impairment, minor speech or linguistic deficits (23–50% of left-sided lesions), attention difficulties, and mood changes or depression (14–33%).[30][36][42][39] Motor weakness is often absent, minor/slight, or transient, and reportedly does not occur with lesions confined exclusively to the caudate nucleus.[30][31] Abulia is defined as decreased spontaneous verbal and motor activity and slowness, with symptoms including apathy, disinterest, flattened affect, lethargy, and lack of initiative for usual daily activities.[36] Cognitive and memory impairment includes poor free recall of episodic and semantic items, verbal amnesia (33% of left-sided lesions), and visual amnesia (right-sided lesions), among other deficits.[30][41][40] Less commonly, there are motor disorders (20–23%), like chorea (6–7%), ballism, tremor, parkinsonism (2–3%), and dystonia (9–16%), as well as more severe cognitive and behavioral problems, like psychic akinesia (loss of psychic self-activation) (12%), neglect (10% with right-sided lesions), aphasia (2–5%), and global dementia (9%, or 1 of 11 and with bilateral lesions).[30][36][41][39] Among strokes in general, and/or among basal ganglia strokes specifically, certain sequelae, including apathy, abulia, fatigue, and depression, have been particularly associated with caudate strokes relative to strokes occurring in other regions.[42][39][48][49][50] Strokes in the caudate nucleus have also been strongly associated with post-stroke restless legs syndrome (RLS).[51][52][53] Other behavioral conditions, like obsessive–compulsive disorder, perseverations, and mania, have been reported rarely in individuals with caudate strokes as well.[12][31][30][54][55] In one case report of bilateral caudate head damage, severe prospective memory impairment was measured, along with other deficits.[12][56]
The sizes, locations, and involvements of neighboring structures define the symptoms of caudate lesions.[41] Damage to the caudate nucleus usually presents with cognitive and behavioral symptoms rather than with neurological signs.[12][30] Cognitive and behavioral symptoms are more common than motor problems (e.g., respective rates of 39% vs. 20% in the 1994 meta-analysis).[42][12][30][39] Due to the predominance of cognitive and behavioral symptoms over neurological symptoms, and frequent absence of classical stroke signs, people with caudate strokes can be misdiagnosed as having primarily psychogenic illness.[34] This can result in enduring cognitive and behavioral deficits, which can result in significant functional limitations, being overlooked.[34] The symptoms of caudate strokes are usually more severe and persistent when they are bilateral rather than unilateral.[31][30] In addition, they are more severe when other adjacent structures are also involved.[31][30] Mendez et al. (1989) categorized caudate stroke patients into three groups based on stroke location and patterns of clinical symptoms: (1) apathetic or abulic, with difficulties perseverating in tasks (dorsolateral caudate); (2) restless, agitated, hyperactive, disinhibited, inappropriate, impulsive, distractible, and/or inattentive (ventromedial caudate); and (3) affective disturbances (anxiety, depression, bipolar disorder) with psychotic features (hallucinations, delusions) (dorsolateral caudate, with larger lesions and more often extending into adjacent areas).[31][30][34] Sometimes, abulia can alternate with periods of disinhibition and agitation in people with caudate strokes.[42][30][31] The symptoms of caudate infarcts are assumed to be due to interruption of neural circuits such as cortico–striatal–thalamic–cortical loops.[31][30][36]
Caudate nucleus hemorrhages can mimic the symptoms of subarachnoid hemorrhage and can include headache, nausea, vomiting, neck stiffness, decreased level of consciousness, hemiparesis, aphasia, neuropsychological disturbances, disorientation, aphasia, mental confusion, and gaze abnormalities, among others.[30][41][42] Caudate hemorrhages are due to rupture of penetrating arteries.[30] Aside from additional acute subarachnoid hemorrhage-like symptoms, symptoms of caudate hemorrhages are similar to those of caudate infarcts, including features like behavioral abnormalities, dysarthria, movement disorders, language disorders, and memory problems.[41]
The prognosis of caudate strokes has been considered good and benign, with majorities of individuals recovering and becoming independent.[41][30] However, patients with caudate strokes can have residual deficits and dependency needs, can worsen clinically with time, or can require institutionalization.[30] Bokura & Robinson (1997) found that some individuals with caudate strokes deteriorated on the mini-mental state examination (MMSE), a short clinical test of basic cognitive function and impairment, during follow-up over 1 to 2 years, whereas patients with other subcortical lesions tended to improve over 2 years.[31][37] People with caudate strokes only rarely die, and generally because of underlying heart disease or other problems rather than the stroke itself.[30] However, although having favorable prognosis in the short-term, and having previously thought to be relatively benign, lacunar strokes in general are associated with greatly increased risk of stroke recurrence, cognitive impairment and dementia, and early death in the mid- to long-term.[57][58][59][60][61] Treatment of caudate strokes may consist of antiplatelet or anticoagulant agents and management of stroke risk factors like hypertension and diabetes mellitus to reduce the risk of additional strokes.[30] On the basis of case reports and small case series, disorders of diminished motivation, like apathy, abulia, and akinetic mutism, secondary to stroke and other causes, may be treated with dopaminergic agents and other pro-motivational medications, including psychostimulants, bupropion, atomoxetine, modafinil, dopamine agonists, levodopa, selegiline, and acetylcholinesterase inhibitors.[62][63][64]
Caudate resection
[edit]The caudate nucleus is sometimes surgically resected to treat glioma that has infiltrated the structure.[65] Opinions in this area are mixed about resecting the caudate, with some authors reporting relatively few deficits upon caudate removal, and others recommending against removal due to poor cognitive and behavioral outcomes, for instance abulia.[65][66][67]
Alzheimer's disease
[edit]A 2013 study has suggested a link between Alzheimer's patients and the caudate nucleus. MRI images were used to estimate the volume of caudate nuclei in patients with Alzheimer's and normal volunteers. The study found a "significant reduction in the caudate volume" in Alzheimer's patients when compared to the normal volunteers. While the correlation does not indicate causation, the finding may have implications for early diagnosis.[68]
Parkinson's disease
[edit]Parkinson's disease is likely the most studied basal ganglia disorder. Patients with this progressive neurodegenerative disorder often first experience movement related symptoms (the three most common being tremors at rest, muscular rigidity, and akathisia) which are later combined with various cognitive deficiencies, including dementia.[69] Parkinson's disease depletes dopaminergic neurons in the nigrostriatal tract, a dopamine pathway that is connected to the head of the caudate. As such, many studies have correlated the loss of dopaminergic neurons that send axons to the caudate nucleus and the degree of dementia in Parkinson's patients.[14] And while a relationship has been drawn between the caudate and Parkinson's motor deficiencies, the caudate has also been associated with Parkinson's concomitant cognitive impairments. One review contrasts the performance of patients with Parkinson's and patients that strictly had frontal-lobe damage in the Tower of London test. The differences in performance between the two types of patients (in a test that, in short, requires subjects to select appropriate intermediate goals with a larger goal in mind) draws a link between the caudate and goal-directed action. However, the studies are not conclusive. While the caudate has been associated with executive function (see "Goal-Directed Action"), it remains "entirely unclear whether executive deficits in [Parkinson's patients] reflect pre-dominantly their cortical or subcortical damage."[14]
Huntington's disease
[edit]In Huntington's disease, a genetic mutation occurs in the HTT gene which encodes for Htt protein. The Htt protein interacts with over 100 other proteins, and appears to have multiple biological functions.[70] The behavior of this mutated protein is not completely understood, but it is toxic to certain cell types, particularly in the brain. Early damage is most evident in the striatum, but as the disease progresses, other areas of the brain are also more conspicuously affected. Early symptoms are attributable to functions of the striatum and its cortical connections—namely control over movement, mood and higher cognitive function.[71]
Attention-deficit hyperactivity disorder
[edit]A 2002 study draws a relationship between caudate asymmetry and symptoms related to ADHD. The authors used MR images to compare the relative volumes of the caudate nuclei (as the caudate is a bilateral structure), and drew a connection between any asymmetries and symptoms of ADHD: "The degree of caudate asymmetry significantly predicted cumulative severity ratings of inattentive behaviors." This correlation is congruent with previous associations of the caudate with attentional functioning.[72] A more recent 2018 study replicated these findings, and demonstrated that the caudate asymmetries related to ADHD were more pronounced in the dorsal medial regions of the caudate.[73]
Schizophrenia
[edit]The volume of white matter in the caudate nucleus has been linked with patients diagnosed with schizophrenia. A 2004 study uses magnetic resonance imaging to compare the relative volume of white matter in the caudate among schizophrenia patients. Those patients with the disorder have "smaller absolute and relative volumes of white matter in the caudate nucleus than healthy subjects."[74]
Bipolar type I
[edit]A 2014 study found Type I Bipolar patients had relatively higher volume of gray and white matter in the caudate nucleus and other areas associated with reward processing and decision making, compared to controls and Bipolar II subjects. Overall the amount of gray and white matter in Bipolar patients was lower than controls.[75][76]
Obsessive-compulsive disorder
[edit]It has been theorized that the caudate nucleus may be dysfunctional in persons with obsessive compulsive disorder (OCD), in that it may perhaps be unable to properly regulate the transmission of information regarding worrying events or ideas between the thalamus and the orbitofrontal cortex.
A neuroimaging study with positron emission tomography found that the right caudate nucleus had the largest change in glucose metabolism after patients had been treated with paroxetine.[77] Recent SDM meta-analyses of voxel-based morphometry studies comparing people with OCD and healthy controls have found people with OCD to have increased grey matter volumes in bilateral lenticular nuclei, extending to the caudate nuclei, while decreased grey matter volumes in bilateral dorsal medial frontal/anterior cingulate gyri.[78][79] These findings contrast with those in people with other anxiety disorders, who evince decreased (rather than increased) grey matter volumes in bilateral lenticular / caudate nuclei, while also decreased grey matter volumes in bilateral dorsal medial frontal/anterior cingulate gyri.[79]
Additional images
[edit]-
Coronal section through anterior cornua of lateral ventricles.
-
Coronal section of brain through anterior commissure.
-
Superficial dissection of brain-stem. Lateral view. The caudate nucleus can be seen above the optic nerve.
-
Dissection of brain-stem. Lateral view.
-
Deep dissection of brain-stem. Lateral view.
-
Deep dissection of brain-stem. Lateral view.
-
Superficial dissection of brain-stem. Ventral view.
-
Dissection of brain-stem. Dorsal view.
-
Central part and anterior and posterior cornua of lateral ventricles exposed from above.
-
Caudate nucleus
-
Caudate nucleus
-
Ventricles of brain and basal ganglia. Superior view, horizontal section, deep dissection
-
Ventricles of brain and basal ganglia. Close-up of preceding image
-
Caudate nuclei along with other subcortical structures, in glass brain
-
Caudate nucleus highlighted in green on coronal T1 MRI images
-
Caudate nucleus highlighted in green on sagittal T1 MRI images
-
Caudate nucleus highlighted in green on transversal T1 MRI images
References
[edit]- ^ a b Yager LM, Garcia AF, Wunsch AM, Ferguson SM (August 2015). "The ins and outs of the striatum: Role in drug addiction". Neuroscience. 301: 529–541. doi:10.1016/j.neuroscience.2015.06.033. PMC 4523218. PMID 26116518.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 147–148. ISBN 9780071481274.
- ^ Bear, Mark F. (2016). Neuroscience : exploring the brain. Connors, Barry W.,, Paradiso, Michael A. (Fourth ed.). Philadelphia. p. 502. ISBN 9780781778176. OCLC 897825779.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 326. ISBN 9780071481274.
Evidence that the caudate nucleus and putamen influence stimulus-response learning comes from lesion studies in rodents and primates and from neuroimaging studies in humans and from studies of human disease. In Parkinson disease, the dopaminergic innervation of the caudate and putamen is severely compromised by the death of dopamine neurons in the substantia nigra pars compacta (Chapter 17). Patients with Parkinson disease have normal declarative memory (unless they have a co-occurring dementia as may occur in Lewy body disease.) However, they have marked impairments of stimulus-response learning. Patients with Parkinson disease or other basal ganglia disorders such as Huntington disease (in which caudate neurons themselves are damaged) have deficits in other procedural learning tasks, such as the acquisition of new motor programs.
- ^ Anderson BA, Kuwabara H, Wong DF, Roberts J, Rahmim A, Brašić JR, Courtney SM (August 2017). "Linking dopaminergic reward signals to the development of attentional bias: A positron emission tomographic study". NeuroImage. 157: 27–33. doi:10.1016/j.neuroimage.2017.05.062. PMC 5600829. PMID 28572059.
- ^ Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 321. ISBN 9780071481274.
Functional neuroimaging in humans demonstrates activation of the prefrontal cortex and caudate nucleus (part of the striatum) in tasks that demand inhibitory control of behavior.
- ^ Yeterian EH, Pandya DN (February 1995). "Corticostriatal connections of extrastriate visual areas in rhesus monkeys". The Journal of Comparative Neurology. 352 (3): 436–57. doi:10.1002/cne.903520309. PMID 7706560. S2CID 42928601.
- ^ D'Souza, Donna. "Cerebral vascular territories - Radiology Reference Article - Radiopaedia.org". radiopaedia.org.
- ^ McDougal, David. "Substantia Nigra". Archived from the original on 30 September 2013. Retrieved 5 December 2013.
- ^ Postle BR, D'Esposito M (July 1999). "Dissociation of human caudate nucleus activity in spatial and nonspatial working memory: an event-related fMRI study". Brain Research. Cognitive Brain Research. 8 (2): 107–15. doi:10.1016/s0926-6410(99)00010-5. PMID 10407200.
- ^ Postle BR, D'Esposito M (June 2003). "Spatial working memory activity of the caudate nucleus is sensitive to frame of reference". Cognitive, Affective, & Behavioral Neuroscience. 3 (2): 133–44. doi:10.3758/cabn.3.2.133. PMID 12943328.
- ^ a b c d e f g Villablanca JR (2010). "Why do we have a caudate nucleus?". Acta Neurobiol Exp (Wars). 70 (1): 95–105. PMID 20407491.
- ^ White NM (April 2009). "Some highlights of research on the effects of caudate nucleus lesions over the past 200 years". Behavioural Brain Research. 199 (1): 3–23. doi:10.1016/j.bbr.2008.12.003. PMID 19111791. S2CID 3717092.
- ^ a b c d e Grahn JA, Parkinson JA, Owen AM (April 2009). "The role of the basal ganglia in learning and memory: neuropsychological studies". Behavioural Brain Research. 199 (1): 53–60. doi:10.1016/j.bbr.2008.11.020. PMID 19059285. S2CID 15685091.
- ^ Elliott R, Newman JL, Longe OA, Deakin JF (January 2003). "Differential response patterns in the striatum and orbitofrontal cortex to financial reward in humans: a parametric functional magnetic resonance imaging study". The Journal of Neuroscience. 23 (1): 303–7. doi:10.1523/JNEUROSCI.23-01-00303.2003. PMC 6742125. PMID 12514228.
- ^ a b Hannan KL, Wood SJ, Yung AR, Velakoulis D, Phillips LJ, Soulsby B, Berger G, McGorry PD, Pantelis C (June 2010). "Caudate nucleus volume in individuals at ultra-high risk of psychosis: a cross-sectional magnetic resonance imaging study". Psychiatry Research. 182 (3): 223–30. doi:10.1016/j.pscychresns.2010.02.006. PMID 20488675. S2CID 35678217.
- ^ Levitt JJ, McCarley RW, Dickey CC, Voglmaier MM, Niznikiewicz MA, Seidman LJ, Hirayasu Y, Ciszewski AA, Kikinis R, Jolesz FA, Shenton ME (July 2002). "MRI study of caudate nucleus volume and its cognitive correlates in neuroleptic-naive patients with schizotypal personality disorder". The American Journal of Psychiatry. 159 (7): 1190–7. doi:10.1176/appi.ajp.159.7.1190. PMC 2826363. PMID 12091198.
- ^ McGaugh JL (2004). "The amygdala modulates the consolidation of memories of emotionally arousing experiences". Annual Review of Neuroscience. 27: 1–28. doi:10.1146/annurev.neuro.27.070203.144157. PMID 15217324.
- ^ Seger CA, Cincotta CM (March 2005). "The roles of the caudate nucleus in human classification learning". The Journal of Neuroscience. 11. 25 (11): 2941–51. doi:10.1523/jneurosci.3401-04.2005. PMC 6725143. PMID 15772354.
- ^ Gogichadze M, Oniani MT, Nemsadze M, Oniani N (2009). "Sleep disorders and disturbances in memory processing related to the lesion of the caudate nucleus". Parkinsonism and Related Disorders. 15: S167 – S168. doi:10.1016/S1353-8020(09)70639-X.
- ^ Villablanca JR (September 2004). "Counterpointing the functional role of the forebrain and of the brainstem in the control of the sleep-waking system". Journal of Sleep Research. 13 (3): 179–208. doi:10.1111/j.1365-2869.2004.00412.x. PMID 15339255.
- ^ Kaufmann C, Wehrle R, Wetter TC, Holsboer F, Auer DP, Pollmächer T, Czisch M (March 2006). "Brain activation and hypothalamic functional connectivity during human non-rapid eye movement sleep: an EEG/fMRI study". Brain. 129 (Pt 3): 655–67. doi:10.1093/brain/awh686. PMID 16339798.
- ^ Kumar R, Ahdout R, Macey PM, Woo MA, Avedissian C, Thompson PM, Harper RM (November 2009). "Reduced caudate nuclei volumes in patients with congenital central hypoventilation syndrome". Neuroscience. 163 (4): 1373–9. doi:10.1016/j.neuroscience.2009.07.038. PMC 2761724. PMID 19632307.
- ^ Ishizu T, Zeki S (May 2011). Warrant EJ (ed.). "Toward a brain-based theory of beauty". PLOS ONE. 6 (7): e21852. Bibcode:2011PLoSO...621852I. doi:10.1371/journal.pone.0021852. PMC 3130765. PMID 21755004.
- ^ Aron A, Fisher H, Mashek DJ, Strong G, Li H, Brown LL (July 2005). "Reward, motivation, and emotion systems associated with early-stage intense romantic love". Journal of Neurophysiology. 94 (1): 327–37. doi:10.1152/jn.00838.2004. PMID 15928068. S2CID 396612.
- ^ Crinion J, Turner R, Grogan A, Hanakawa T, Noppeney U, Devlin JT, Aso T, Urayama S, Fukuyama H, Stockton K, Usui K, Green DW, Price CJ (June 2006). "Language control in the bilingual brain". Science. 312 (5779): 1537–40. Bibcode:2006Sci...312.1537C. doi:10.1126/science.1127761. PMID 16763154. S2CID 10445511.
- ^ "How bilingual brains switch between tongues". newscientist.com.
- ^ Newberg AB, Wintering NA, Morgan D, Waldman MR (November 2006). "The measurement of regional cerebral blood flow during glossolalia: a preliminary SPECT study". Psychiatry Research. 148 (1): 67–71. doi:10.1016/j.pscychresns.2006.07.001. PMID 17046214. S2CID 17079826.
- ^ Braitenberg V. (1984) Vehicles. Experiments in synthetic psychology.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae Chung, Chin-Sang; Caplan, Louis R. (2012-07-12). "Caudate nucleus infarcts and hemorrhages". In Caplan, Louis R.; van Gijn, Jan (eds.). Stroke syndromes (3 ed.). Cambridge: Cambridge University Press. pp. 397–404. doi:10.1017/cbo9781139093286.034. ISBN 978-1-139-09328-6.
- ^ a b c d e f g h i j k l m n o p q Caplan, L R (2002-04-11). "Caudate infarcts". Subcortical Stroke. Oxford University PressNew York, NY. pp. 209–224. doi:10.1093/oso/9780192631572.003.0018. ISBN 978-0-19-263157-2.
- ^ Stein RW, Kase CS, Hier DB, Caplan LR, Mohr JP, Hemmati M, Henderson K (December 1984). "Caudate hemorrhage". Neurology. 34 (12): 1549–54. doi:10.1212/wnl.34.12.1549. PMID 6504325.
- ^ Weisberg LA (September 1984). "Caudate hemorrhage". Arch Neurol. 41 (9): 971–4. doi:10.1001/archneur.1984.04050200077021. PMID 6477232.
- ^ a b c d Mendez MF, Adams NL, Lewandowski KS (March 1989). "Neurobehavioral changes associated with caudate lesions". Neurology. 39 (3): 349–54. doi:10.1212/wnl.39.3.349. PMID 2927642.
- ^ Caplan LR, Schmahmann JD, Kase CS, Feldmann E, Baquis G, Greenberg JP, Gorelick PB, Helgason C, Hier DB (February 1990). "Caudate infarcts". Arch Neurol. 47 (2): 133–43. doi:10.1001/archneur.1990.00530020029011. PMID 2405818.
- ^ a b c d e f g h Caplan, L. R.; Helgason, C. M. (1995). "Caudate infarcts". In Donnan, G. A.; Norrving, B.; Bamford, J. M.; Bogousslavsky, J. (eds.). Lacunar and Other Subcortical Infarctions. Oxford: Oxford University Press. pp. 117–130.
- ^ a b Bokura H, Robinson RG (May 1997). "Long-term cognitive impairment associated with caudate stroke". Stroke. 28 (5): 970–5. doi:10.1161/01.str.28.5.970. PMID 9158635.
- ^ a b c Kumral E, Evyapan D, Balkir K (January 1999). "Acute caudate vascular lesions". Stroke. 30 (1): 100–8. doi:10.1161/01.str.30.1.100. PMID 9880396.
- ^ a b c d e f g Gnanashanmugam, G. (2011). A Study on Evaluation of Motor, Cognitive and Behavioral Manifestations of Basal Ganglia Infarcts (Doctoral dissertation, Madras Medical College, Chennai). http://repository-tnmgrmu.ac.in/id/eprint/580
- ^ a b Kumral E, Çetin FE, Özdemir HN (2023). "A Neuropsychiatric and Neuroimaging Study of Unilateral and Bilateral Striatal Ischemic Lesions". J Neuropsychiatry Clin Neurosci. 35 (1): 48–58. doi:10.1176/appi.neuropsych.21030083. PMID 35872616.
- ^ a b c d e f g h i j k Pellizzaro Venti, Michele; Paciaroni, Maurizio; Caso, Valeria (2012). "Caudate Infarcts and Hemorrhages". In Paciaroni, M.; Agnelli, G.; Caso, V.; Bogousslavsky, J. (eds.). Frontiers of Neurology and Neuroscience. Vol. 30. S. Karger AG. pp. 137–140. doi:10.1159/000333616. ISBN 978-3-8055-9910-8.
- ^ a b c d e f g h i j Bhatia KP, Marsden CD (August 1994). "The behavioural and motor consequences of focal lesions of the basal ganglia in man". Brain. 117 ( Pt 4) (4): 859–76. doi:10.1093/brain/117.4.859. PMID 7922471.
- ^ Grönholm EO, Roll MC, Horne MA, Sundgren PC, Lindgren AG (January 2016). "Predominance of caudate nucleus lesions in acute ischaemic stroke patients with impairment in language and speech". Eur J Neurol. 23 (1): 148–53. doi:10.1111/ene.12822. PMC 5042068. PMID 26268364.
The occurrence of stroke involving only the caudate nucleus seems overall rather uncommon. In one register study 23, it was reported that patients with caudate stroke constituted only 1% of a total number of 3050 stroke patients (2450 ischaemic stroke and 600 haemorrhagic stroke). In the present study, at least nine of the 925 patients initially included in the investigation had lesions involving an area in the superior part of the body of the left caudate nucleus and the adjacent corona radiata.
- ^ Gerraty RP (September 2003). "Clinical diagnosis of subcortical cerebral infarction". Expert Rev Neurother. 3 (5): 703–11. doi:10.1586/14737175.3.5.703. PMID 19810969.
Clinical diagnosis of subcortical infarction, chiefly lacunar stroke, [...] Subcortical infarction is unfortunately often considered synonymous with lacunar stroke, [...] Not all subcortical strokes are lacunes. The large striatocapsular infarct, even though confined to subcortical structures, usually does give cortical signs [3,4]. The smaller restricted striatocapsular infarct, also due to embolism as is the larger variety, usually does not give cortical signs and is an underacknowledged entity [5,6]. There are other subcortical strokes, including internal borderzone (watershed) infarction, considered most likely due to hypoperfusion and others with even less certain patho-etiologies (TABLE 1) [5,7].
- ^ Weiller, C. (2002). "Striatocapsular infarcts". In Donnan, G. (ed.). Subcortical Stroke. Oxford medical publications. Oxford University Press. pp. 195–208. ISBN 978-0-19-263157-2. Retrieved 9 December 2023.
- ^ Godfrey J (March 2009). "Safety of therapeutic methylphenidate in adults: a systematic review of the evidence". J Psychopharmacol. 23 (2): 194–205. doi:10.1177/0269881108089809. PMID 18515459.
- ^ Sadeghian H (February 2004). "Lacunar stroke associated with methylphenidate abuse". Can J Neurol Sci. 31 (1): 109–11. doi:10.1017/s0317167100002924. PMID 15038480.
- ^ Tang, W.K.; Liang, H.J.; Chen, Y.K.; Chu, Winnie C.W.; Abrigo, Jill; Mok, V.C.T.; Ungvari, Gabor S.; Wong, K.S. (2013). "Poststroke fatigue is associated with caudate infarcts". Journal of the Neurological Sciences. 324 (1–2): 131–135. doi:10.1016/j.jns.2012.10.022.
- ^ Riahi, A., Derbali, H., Bedoui, I., Messelmani, M., Mansour, M., Zaouali, J., & Mrissa, R. (2016, June). Implication of Caudate nucleus lacunar infarcts in post-stroke depression. European Journal of Neurology, 23(Suppl 2), 756–756 (abstract no. P32016). https://doi.org/10.1111/ene.13094
- ^ Riggi, F. F., Hommel, M., & Jaillard, A. (2018). Lesions in the dorsolateral caudate nucleus predict post stroke depression – a voxel-based lesion-symptom mapping study. Cerebrovascular Diseases, 45(Suppl 1), 33–33 (abstract no. OP 025). https://doi.org/10.1159/000520354
- ^ Wang XX, Feng Y, Tan EK, Ondo WG, Wu YC (February 2022). "Stroke-related restless legs syndrome: epidemiology, clinical characteristics, and pathophysiology". Sleep Med. 90: 238–248. doi:10.1016/j.sleep.2022.02.001. PMID 35219214.
- ^ Wu X, Xu J, Lu B (June 2020). "Acute post-stroke restless legs syndrome: the body of caudate nucleus considerations". Sleep Med. 70: 66–70. doi:10.1016/j.sleep.2019.11.1253. PMID 32229419.
- ^ Ruppert E, Hacquard A, Tatu L, Namer IJ, Wolff V, Kremer S, Lagha-Boukbiza O, Bataillard M, Bourgin P (April 2022). "Stroke-related restless legs syndrome: Clinical and anatomo-functional characterization of an emerging entity". Eur J Neurol. 29 (4): 1011–1016. doi:10.1111/ene.15207. PMID 34889000.
- ^ Akaho R, Deguchi I, Kigawa H, Nishimura K (April 2019). "Obsessive-Compulsive Disorder Following Cerebrovascular Accident: A Case Report and Literature Review". J Stroke Cerebrovasc Dis. 28 (4): e17 – e21. doi:10.1016/j.jstrokecerebrovasdis.2018.12.034. PMID 30638936.
- ^ Satzer D, Bond DJ (May 2016). "Mania secondary to focal brain lesions: implications for understanding the functional neuroanatomy of bipolar disorder". Bipolar Disord. 18 (3): 205–20. doi:10.1111/bdi.12387. PMID 27112231.
- ^ Canavero S, Fontanella M (1998). "Behavioral-attentional syndrome following bilateral caudate head ischaemia". J Neurol. 245 (6–7): 322–4. doi:10.1007/s004150050226. PMID 9669482.
- ^ Arboix A, Martí-Vilalta JL (February 2009). "Lacunar stroke". Expert Rev Neurother. 9 (2): 179–96. doi:10.1586/14737175.9.2.179. PMID 19210194.
Lacunar infarcts show a paradoxical clinical course with a favorable prognosis in the short term, characterized by a low early mortality and reduced functional disability on hospital discharge, but with an increased risk of death, stroke recurrence and dementia in the mid- and long term. Asymptomatic progression of small-vessel disease is a typical feature of the lacunar infarcts. For this reason, lacunar infarction should be regarded as a potentially severe condition rather than a relatively benign disorder and, therefore, lacunar stroke patients require adequate and rigorous management and follow-up.
- ^ Gore M, Bansal K, Khan Suheb MZ, Asuncion RM (2024). "Lacunar Stroke". PMID 33085363.
In a follow-up study, patients with lacunar infarcts are diagnosed with dementia 4 to 12 times more frequently than the average population.[15] Post-stroke dementia in accumulated lacunar infarct is common despite their small size and association with small vessel disease.[16] [...] Lacunar strokes are a common cause of vascular dementia and mild cognitive impairment, often overlooked in clinical practice. Multiple silent lacunar strokes are documented on brain MRI, with patients presenting with mild cognitive impairment and early dementia.[32]
- ^ Norrving B (August 2008). "Lacunar infarcts: no black holes in the brain are benign". Pract Neurol. 8 (4): 222–8. doi:10.1136/jnnp.2008.153601. PMID 18644908.
Recent studies have shown that the prognosis after lacunar infarcts is not benign; the risk of recurrent stroke is no lower than for other ischaemic stroke subtypes, and there is an increased risk for cognitive decline, dementia and death in the long term.
- ^ Norrving B (April 2003). "Long-term prognosis after lacunar infarction". Lancet Neurol. 2 (4): 238–45. doi:10.1016/s1474-4422(03)00352-1. PMID 12849212.
[Lacunar] infarcts have commonly been regarded as benign vascular lesions with a favourable long-term prognosis. However, recent studies have shown that this is only the case early in the disease course. A few years after infarct, there is an increased risk of death, mainly from cardiovascular causes. The risk of recurrent stroke after lacunar infarct is similar to that for most other types of stroke, and patients have an increased risk of developing cognitive decline and dementia.
- ^ Grau-Olivares M, Arboix A (August 2009). "Mild cognitive impairment in stroke patients with ischemic cerebral small-vessel disease: a forerunner of vascular dementia?". Expert Rev Neurother. 9 (8): 1201–17. doi:10.1586/ern.09.73. PMID 19673608.
- ^ Marin RS, Wilkosz PA (2005). "Disorders of diminished motivation". J Head Trauma Rehabil. 20 (4): 377–88. doi:10.1097/00001199-200507000-00009. PMID 16030444.
- ^ Spiegel DR, Warren A, Takakura W, Servidio L, Leu N (January 2018). "Disorders of diminished motivation: What they are, and how to treat them" (PDF). Current Psychiatry. 17 (1): 10–18, 20.
- ^ Arnts H, van Erp WS, Lavrijsen JC, van Gaal S, Groenewegen HJ, van den Munckhof P (May 2020). "On the pathophysiology and treatment of akinetic mutism". Neurosci Biobehav Rev. 112: 270–278. doi:10.1016/j.neubiorev.2020.02.006. hdl:2066/225901. PMID 32044373.
- ^ a b Çırak M, Yağmurlu K, Kearns KN, Ribas EC, Urgun K, Shaffrey ME, Kalani MY (July 2020). "The Caudate Nucleus: Its Connections, Surgical Implications, and Related Complications". World Neurosurg. 139: e428 – e438. doi:10.1016/j.wneu.2020.04.027. PMID 32311569.
- ^ Duffau H, Denvil D, Capelle L (August 2002). "Absence of movement disorders after surgical resection of glioma invading the right striatum". J Neurosurg. 97 (2): 363–9. doi:10.3171/jns.2002.97.2.0363. PMID 12186465.
- ^ Müller DM, Robe PA, Eijgelaar RS, Witte MG, Visser M, de Munck JC, Broekman ML, Seute T, Hendrikse J, Noske DP, Vandertop WP, Barkhof F, Kouwenhoven MC, Mandonnet E, Berger MS, De Witt Hamer PC (January 2019). "Comparing Glioblastoma Surgery Decisions Between Teams Using Brain Maps of Tumor Locations, Biopsies, and Resections". JCO Clin Cancer Inform. 3 (3): 1–12. doi:10.1200/CCI.18.00089. PMC 6873995. PMID 30673344.
- ^ Jiji S, Smitha KA, Gupta AK, Pillai VP, Jayasree RS (September 2013). "Segmentation and volumetric analysis of the caudate nucleus in Alzheimer's disease". European Journal of Radiology. 82 (9): 1525–30. doi:10.1016/j.ejrad.2013.03.012. PMID 23664648.
- ^ Kolb, Bryan; Ian Q. Whishaw (2001). An Introduction to Brain and Behavior (4th ed.). New York: Worth Publishers. p. 590. ISBN 978-1429242288.
- ^ Goehler H, Lalowski M, Stelzl U, Waelter S, Stroedicke M, Worm U, Droege A, Lindenberg KS, Knoblich M, Haenig C, Herbst M, Suopanki J, Scherzinger E, Abraham C, Bauer B, Hasenbank R, Fritzsche A, Ludewig AH, Büssow K, Buessow K, Coleman SH, Gutekunst CA, Landwehrmeyer BG, Lehrach H, Wanker EE (September 2004). "A protein interaction network links GIT1, an enhancer of huntingtin aggregation, to Huntington's disease". Molecular Cell. 15 (6): 853–65. doi:10.1016/j.molcel.2004.09.016. PMID 15383276.
- ^ Walker FO (January 2007). "Huntington's disease". Lancet. 369 (9557): 218–28. doi:10.1016/S0140-6736(07)60111-1. PMID 17240289. S2CID 46151626.
- ^ Schrimsher GW, Billingsley RL, Jackson EF, Moore BD (December 2002). "Caudate nucleus volume asymmetry predicts attention-deficit hyperactivity disorder (ADHD) symptomatology in children". Journal of Child Neurology. 17 (12): 877–84. doi:10.1177/08830738020170122001. PMID 12593459. S2CID 36086945.
- ^ Douglas PK, Gutman B, Anderson A, Larios C, Lawrence KE, Narr K, Sengupta B, Cooray G, Douglas DB, Thompson PM, McGough JJ, Bookheimer SY (February 2018). "Hemispheric brain asymmetry differences in youths with attention-deficit/hyperactivity disorder". NeuroImage: Clinical. 18: 744–52. doi:10.1016/j.nicl.2018.02.020. PMC 5988460. PMID 29876263.
- ^ Takase K, Tamagaki C, Okugawa G, Nobuhara K, Minami T, Sugimoto T, Sawada S, Kinoshita T (2004). "Reduced white matter volume of the caudate nucleus in patients with schizophrenia". Neuropsychobiology. 50 (4): 296–300. doi:10.1159/000080956. PMID 15539860. S2CID 7921315. ProQuest 293981781.
- ^ Maller, Jerome J.; Thaveenthiran, Prasanthan; Thomson, Richard H.; McQueen, Susan; Fitzgerald, Paul B. (2014). "Volumetric, cortical thickness and white matter integrity alterations in bipolar disorder type I and II". Journal of Affective Disorders. 169: 118–127. doi:10.1016/j.jad.2014.08.016. PMID 25189991.
- ^ "A Trip Into Bipolar Brains". psmag.com. 14 June 2017.
- ^ Hansen ES, Hasselbalch S, Law I, Bolwig TG (March 2002). "The caudate nucleus in obsessive-compulsive disorder. Reduced metabolism following treatment with paroxetine: a PET study". The International Journal of Neuropsychopharmacology. 5 (1): 1–10. doi:10.1017/S1461145701002681. PMID 12057027.
- ^ Radua J, Mataix-Cols D (November 2009). "Voxel-wise meta-analysis of grey matter changes in obsessive-compulsive disorder". The British Journal of Psychiatry. 195 (5): 393–402. doi:10.1192/bjp.bp.108.055046. PMID 19880927.
- ^ a b Radua J, van den Heuvel OA, Surguladze S, Mataix-Cols D (July 2010). "Meta-analytical comparison of voxel-based morphometry studies in obsessive-compulsive disorder vs other anxiety disorders". Archives of General Psychiatry. 67 (7): 701–11. doi:10.1001/archgenpsychiatry.2010.70. PMID 20603451.


















